Many symptoms of MS are invisible while others are painfully obvious. All can impact on quality of life and sense of wellbeing. While life changes affect everyone, changes from MS can directly and indirectly affect sexuality. Successful management requires creativity, communication, patience and resource management so that a person is able to maintain his or her sexual identity.
Sexual changes in MS can best be characterised as primary, secondary, or tertiary in nature.
Female sexual dysfunction is very common in women with neurological conditions, including MS. The majority of women with MS suffer from sexual dysfunction at some stage of the condition. This is estimated to be as high as 80 per cent, compared to the general female population, in which only 20-50 percent of women are affected. Sexual dysfunction has a major impact on quality of life and interpersonal relationships. For many women it is a physically disquieting, emotionally disturbing and socially disruptive disorder. In spite of its high prevalence, these aspects of an individual’s wellbeing have been considerably neglected until recently, making female sexual dysfunction a very important but often overlooked symptom of MS.
How the body behaves during the sexual response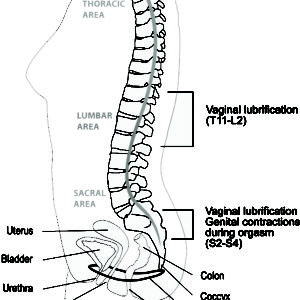
Two basic physical processes occur during the sexual response: vasocongestion and myotonia.
Vasocongestion refers to the concentration of blood in the blood vessels and the tissues of the genitals and breasts. In women, this inflow of blood causes the clitoris to enlarge,the labia to swell, and the vagina to lubricate.
Myotonia or neuromuscular tension, refers to the increase of energy in the nerves and muscles. During sexual activity, myotonia takes place throughout the body, not only in the genital region, but throughout the trunk, particularly in the breast and chest wall.
For women, vasocongestion in the vaginal walls causes vaginal secretion to seep through the vaginal lining, moistening the inner surface of the vagina. The amount of lubrication or “wetness” present in the vagina does not necessarily coincide with a woman’s degree of arousal or desire for intercourse. Swelling of the clitoris and of the labia also occurs in response to vasocongestion during the excitement phase. In addition, the inner two-thirds of the vagina lengthens and expands, the cervix and uterus elevate, and the outer lips of the vagina flatten and separate. Nipples may become erect, breasts slightly enlarged, and the veins in the breasts may appear more visible.
How and why MS can affect sexual functioning
Sexual dysfunction in women has many causes and effects:
Types and frequencies
It is known that approximately 80 per cent of women with MS experience sexual dysfunction at some time during the course of the disease. Some women just stop engaging in sexual relations, while others (approximately 40 per cent) have reported that participating in sexual relations is significantly unsatisfactory.
Symptoms most commonly reported include:
Managing loss of sexual response
Where sensation is disturbed in the genitals or lower body areas, there are simple and practical things you can do. You could start by creating a sensory “body map” with your partner and explore the exact locations of pleasant, decreased, or altered sensations. This involves systematically touching the body from head to toe (or all those places one can comfortably reach). By varying the rate, rhythm, and pressure of touch, you can then be aware of the areas of sensual pleasure. Thereafter, altering the pattern of touch subsequently in these areas can maximise pleasure. Instructing your sexual partner to touch in a similar manner sets the stage for rediscovering sensual and erotic pleasure. Increasing stimulation to erogenous zones, such as breasts, ears, and lips may enhance your orgasmic response. Increasing cerebral stimulation by watching sexually oriented videos, exploring fantasies, and introducing new kinds of sexual play into sexual activities can sometimes promote an orgasmic response. Experimentation and communication are the keys to maximising sexual response and/or pleasure. Where diminished genital sensation occurs, you can increase stimulation through oral stimulation or use mechanical vibrators, which are widely available by mail order online. Painful or irritating genital or body sensations can be relieved with medication. Amitriptyline (Amitrip®), carbamazepine (Tegretol®) and phenytoin (Dilantin®) can be prescribed to help manage this. It is not yet clear how helpful oral medicines like Viagra or cialis could be for women with MS. These are targeted at sexual dysfunction in men to increase blood flow to the genitals.
Lowered libido
Loss of sex drive, or libido, can be a frequent sexual symptom among women with MS. There are currently no effective medicines in New Zealand. However, there are reports that sex therapy combined with MS symptom management and communication skills training, can be successful. This involves re-training behaviour, targeting the rekindling of sexual pleasure, aimed at creating a different set of behaviours and attitudes to arouse sexual pleasure. Even when libido is not present, the nervous system can still be sufficiently intact to respond to sexual stimulation.
Vaginal dryness and tightness
Vaginal lubrication may be compromised by MS. The best way to cope with vaginal dryness is to apply liberal amounts of water-based lubricants (e.g., k-Y® Jelly). It is thought that most women who use a lubricant, may not use it in sufficient amounts. If dryness still persists even after lubricant use, apply more. Oestrogen creams may be useful for women experiencing vaginal dryness, pain or burning. Another treatment is a vaginal suppository. Ask your GP or pharmacist about what is best for you.
Clinical assessment
Since the sexual response in women with MS is related to many different factors, a comprehensive assessment of all these aspects must be taken into account. An evaluation should consist of a full medical history, physical examination and pelvic examination. Although sexual dysfunction in women with MS often has a neurological cause, its evaluation may not always be included in routine clinical practice. Sometimes it is possible for a clinician to only find out about the problem during a visit based on information supplied by the person with MS, and only then begin to evaluate and treat the problem. Initiating these questions is not always part of a healthcare professional’s routine, with the result that important information can be missed and problems experienced by the person with MS left unaddressed. Be sure to mention any problems you may be experiencing to be sure you can access the right help.
Conclusion
Sexual dysfunction is highly prevalent among women with MS. While identification, assessment and treatment of sexual problems can be embarrassing and complicated, addressing them is important. In this way you can identify and manage the symptoms that can have a negative impact on your personal life as well as that of your partner.
Sexual activity for men usually requires the co-ordination of arousal, penile erection and orgasm including ejaculation, along with the many other emotional and relationship components that are integral for satisfaction. Direct disruption of nerve pathways controlling erection and ejaculation are common.
Erectile dysfunction
An erection occurs when there is relaxation of the muscle cells in the wall of the penile blood vessels and the erectile tissue, leading to the penis filling with blood. Relaxation of these muscle cells is initiated by nitric oxide (NO) release from nerves coming from the lower spinal cord. The messages transmitted by these nerves usually arise in the brain and pass down to the lower spinal cord. Erectile dysfunction (ED) is the commonest sexual dysfunction in men and usually is due to a disease of the vascular or neurological systems, but psychosexual influences are also important. ED can have a major impact on self-esteem, relationships and general well being. In men with MS, lesions in the spinal cord that interfere with the passage of nerve impulses from the brain may cause ED. The limited studies of men with MS indicate that ED is a frequent symptom, often affecting younger men and sometimes affecting fertility.
Possible treatments
If you are a man with MS, let your neurologist, gP or MS Nurse know if you are having any erectile dysfunction. If you talk to them about it, its impact can be assessed and, if it is considered significant, a full range of treatment options can then be discussed with you. Treatment is usually erection-promoting medications rather than treating the underlying disorder. Drugs used to modify MS progression may also help. The most commonly-used medications act to enhance the relaxation of muscle cells in the penis. Sildenafil, tadalafil and vardenafil all act in this way through a similar mechanism. They are generally safe, well-tolerated medications and observation of their use in MS and spinal cord injury confirm a high efficacy, with about three-quarters of men experiencing satisfactory outcomes. Education about how to achieve the best results, patience and perseverance are the most important aspects of the use of these medications. They need to be taken at least half an hour before sex, but some couples find the idea of premeditating their sexual experience off-putting, and this often interferes with treatment. Normal sexual stimulation is required to initiate the erection, therefore the couple needs to be in the mood for sex. Apprehension about the outcome may result in less than optimal results for the first few doses. Persistence, medical review and re-instruction are important for successful results.
Side effects
Generally safe, these drugs may cause mild headaches, flushing, nasal congestion, indigestion and muscle aches, but these side effects usually do not preclude their use. When the drug sildenafil was launched, much was said of possible adverse cardiac effects and this may still worry some men and their partners. There is a potentially harmful reaction with all these drugs when used with nitrates (mainly used to treat angina), and men with active heart disease, for whom the level of physical activity during sexual intercourse is potentially dangerous, should use these drugs with caution.
Alternative treatments
If these drugs do not work or cannot be safely used, injecting drugs into the penis or the use of mechanical aides may be helpful. Prostaglandin E1 can be injected directly into the penis. This relaxes the muscle cells and usually induces a hard, lasting erection. Significant dexterity and common sense are essential for self-injection. Penile pain, nodular scarring within the erectile bodies and unduly prolonged erection may occur. The dosing regimen prescribed must be followed strictly. Some men with partial ED can obtain a good erection using a penile ring, usually combined with a vacuum device. The latter draws more blood into the penis while the ring, applied after blood flow into the penis is sufficient, reduces blood flow out of the penis. If all else fails, a penile prosthesis can be implanted so that cylinders implanted into the shaft of the penis can be filled from a fluid reservoir in the scrotum.
Ejaculatory dysfunction
At ejaculation there is widespread muscle contraction in the pelvic area that leads to expulsion of the semen and much of the sensation associated with the broader response of orgasm. These responses are also triggered by nerve impulses that traverse the spinal cord from important brain centres. Often, delayed ejaculation and complete failure of ejaculation (anejaculation) are caused by disruption of the nerve pathways and may be part of a broader orgasmic failure. Ejaculatory disturbances also occur in MS, although there is less information about the prevalence. Anti-depressant medications (see page 31) that may be used in MS often cause ejaculatory problems as a side-effect. Some men with MS may develop premature ejaculation because of anxiety about their disease.
Sexual desire
Testosterone is active in several brain centres important for sexual thoughts and desire (libido) and low levels of it are associated with depression and obesity, both of which can relate to MS. Frequently, desire is affected by factors other than the direct physical component of the disease, and this is particularly so in MS where other physical and psychological factors, such as fatigue, may play a major role.
Possible treatments
Unlike ED, there is no medication that acts directly to improve ejaculatory problems or low desire. Emphasis will be on optimising physical and emotional wellbeing. The ED drugs are often tried where there is difficulty achieving ejaculation and orgasm, as there is often a degree of ED as well. In addition, there is usually heightened stimulation with a harder erection. Also: Different positions help some men to be more stimulated and some benefit from mechanical assistance, e.g. a vibrator. Couples should be reassured that satisfying sex can be achieved without full erection and penetration, and that satisfaction can be achieved by a variety of stimulating techniques.
The male menopause
You’ve probably heard of the menopause in women, but did you know men go through a similar hormonal change as they age? The male menopause, or andropause, is often triggered when men reach their 40s.
In fact, as many as 30% of men can expect some sort of physical change to their bodies when they reach this age. But with such little exposure to information, this sudden shift in mental attitude and physical ability can come as a real shock.
In this guide, Optimale discuss all aspects of the male menopause. From spotting the early signs, to finding out what you can do to alleviate the symptoms, find out what you can do to tackle the challenges of the andropause.
Clinical assessment
Not all men with ED (or even health professionals) find it easy to talk about it, and they may not raise this distressing issue. It is important to note that sexual dysfunction is diagnosed by taking a careful history; there are no diagnostic tests. Men with MS may have other causes of sexual dysfunction and the assessment should take this into account. Simple blood tests to exclude diabetes, high cholesterol and testosterone deficiency are recommended. Careful assessment of the impact of medications and substance use is important. The importance of assessing both the man with MS and his partner cannot be over-emphasised, particularly if initial treatment is not successful. This will require more developed skills that not all doctors will have. Your doctor may be able to refer you to another professional for further help.
MS changes can affect sexual response by making sexual activity difficult physically and emotionally. Symptoms common to MS, such as fatigue or changes in muscle tone, lack of coordination or pain, can frustrate sexual expression and extinguish desire. Bowel and bladder dysfunction can inhibit and cause embarrassment. cognitive changes challenge the most devoted couple, yet in the presence of any of these symptoms, it is possible to find creative ways to keep the physical expressions of love alive. A person who does not feel well or thinks of himself or herself as unattractive because of a less-than-perfect body may shun sex or find their love life deteriorating. People who are not in a relationship may be reluctant to date and develop new love interests. Secondary sexual dysfunction often indirectly affects sexual response and ability to perform in both men and women with MS. Sexual complaints are common in the general population and are capable of having a profound impact on quality of life and relationships. Adding chronic illness to the picture makes problems more likely, yet such concerns and complaints are not always shared with partners or health care professionals. Nevertheless, strategies exist which can be employed to cope with and manage symptoms, promote intimacy, strengthen relationships and encourage sexual pleasure and expression.
This is perhaps the most common symptom reported by people with MS, and it can be the most disabling. Regardless of the type or cause of fatigue, it can have a negative affect on interest in sex and lead to a reluctance to initiate lovemaking, or even an avoidance of intimacy. The well partner may misunderstand this “disinterest” and loss of pleasure and resent the person with MS. This may come at a time when they are assuming additional responsibilities, coping with changing roles or it may be perceived as a personal rejection. Often, partners fear hurting the person with MS. Effective communication requires that feelings be shared and dealt with openly and honestly, thus making it possible to explore options for maintaining a satisfactory sexual relationship despite physical changes.
What you can do
Muscle weakness may necessitate alterations in sexual practices.
What you can do
Lack of coordination may make sex and sexual expression feel clumsy, as can tremor. But besides being awkward, these symptoms may also interfere with the couple’s style of having sex. It must be remembered that persons with MS still have needs for contraception and protection from sexually transmitted disease, but previously-used methods may no longer be practical.
What you can do
Another source of anxiety and distress can be bowel and bladder disturbances. These problems go hand in hand with sexual dysfunction, since nerve pathways are shared or close to each other. Incontinence, or even fear of having an accident, can cause a person to avoid sex entirely, thus depriving them of the closeness it brings.
What you can do
There are many ways to deal with involuntary elimination:
This can impact significantly on interest in sex as well as performance ability. Understanding the type of pain can influence the best way to manage it. Muscle tightness, intense itching and spasticity may all be called “pain”. Also, medications used to relieve pain may add to sleepiness or fatigue.
What you can do
Changes in sensation can also interfere with sexual pleasure. Non-genital symptoms such as numbness and tingling can distract and discourage either partner. Impaired genital sensations can diminish pleasure, while heightened sensitivity may make even the lightest touch unbearable. What feels good at one time may be excruciatingly painful on another occasion.
What you can do
Mobility devices used to compensate for loss of function can also damage your confidence and self-image. They may be seen as less than sexy. Canes, wheelchairs, braces and walkers are often identified with being “sick” or “old”. Spontaneity can be a problem if great effort has to be made to get about.
What you can do
Cognitive changes can be amongst the most potentially damaging to the relationship, since they can undermine the person’s sense of who he/she is. A partner may feel this is no longer the person they once knew. changes in attention and concentration may be perceived as lack of interest or love, and may irreparably strain the relationship. changes in mood, memory loss and depression can be frightening, frustrating and sometimes infuriating. All interfere with intimacy. Individual or couples counselling may be advised.
What you can do
Sexuality is an evolving, overall development of one’s feelings of personal identity, wellbeing and self-esteem that involves both social and physical relationships. This is an individual lifelong process, which is influenced significantly by personal perception, social conditioning, cultural and religious factors.
The onset of MS can alter a person’s perception of himself or herself as an individual, altering sexual development and expressions of sexuality and it can have a negative impact on sexual and intimate functioning. These are known as the tertiary sexual problems of MS, derived from the resultant psychological and social changes, as distinct from the direct neurological dysfunction (primary sexual problems) and the symptoms of MS (secondary sexual problems). Whilst MS is not a disease of the whole person, it can overwhelm and challenge the perception of “self” with negative outcomes in relation to sexuality and sexual functioning. People with MS can find it difficult to see themselves as being “sexual”, having sexual thoughts, desires and needs whilst at the same time identifying with the role of a person with a chronic illness.
Individuals see themselves as complete persons in terms of their roles within families, friendship circles, sporting clubs, activities and occupations. Any feelings of loss of control over events or unplanned changes because of MS can affect one’s confidence and self-esteem and alter the dynamics of relationships, especially close and intimate ones.
The diagnosis of MS, combined with the unpredictable nature of relapses and the uncertainty of disease progression, often occurs at a time when dreams and plans for the future are being formulated and relationships and careers established. The diagnosis of MS may well cloud an individual’s expectation of the future. This can result in reactions of grief, anxiety and depression, lowering self-esteem and reducing confidence. Such feelings may cause reduced sexual interest and withdrawal from sexual activity. The fear of potential or actual disability can have a negative impact on the perception of body image. People with MS may feel less sexual or sexually attractive. This is particularly evident in cultures where desirability is associated with beauty, fitness and health. Sexual feelings and sexual activity are not just for those who are young and able-bodied, yet this is the message continually transmitted by the media.
Increasing disability can bring with it changes in domestic routines, reduction or cessation of employment and reduced social interaction. This can be very distressing for those who have seen their primary role as the wage earner or the homemaker, for example. Disability can also lead to dependency on others for personal care. If the partner provides this care it can be very difficult to separate the role of carer from that of intimate lover. Visiting carers, nursing and domestic services intruding into the home can leave people with MS feeling exposed in all areas of their life, with little private time. Dealing with the impact of MS and symptoms can leave one neglecting the emotional and psychological aspects of life in general. Simply attending to the physical needs of life’s daily activities can leave little time or energy for emotional contemplation and intimate relationships. This is particularly evident if fatigue is experienced as a symptom of the MS. It is important to remember that people with MS are not isolated and living in a vacuum; their worries and concerns affect others. Conflict can become apparent in established relationships if these factors are not recognised and addressed with ongoing and honest communication. Not uncommonly, resulting misunderstanding, resentment and feelings of rejection by the partner occur as they see MS becoming the dominant focus.
What you can do
In order to discuss this important topic effectively while minimising feelings of anxiety and embarrassment as much as possible. There are no rules for whose “job” it is to discuss sexual problems, so talk to the healthcare professional with whom you feel most comfortable. Remember that there is probably a solution to your problem. You do not wait until you reach a crisis to discuss problems. Write down any questions you have between visits, so as not to forget them. Keep an updated list of medications to review during each visit, as a number of medications can negatively influence sexual functioning. Ask your healthcare provider for written material that you can read on your own and discuss later.
It may also be of benefit to seek further help relating to problems of sexuality from health professionals. Whilst bringing up the topic can be difficult and embarrassing, this can also be so for some doctors and health professionals. It is important to find an MS healthcare provider with whom one feels comfortable, or seek a referral to someone specialising in this area. going together, and with pre-written questions, can be helpful and provide the focus for initial consultation.
For health professionals, the key to managing tertiary sexual problems in MS is firstly to identify what issues are having a negative impact on the wellbeing and sexuality of the individual. This includes identification of primary and secondary sexual problems, as well as the psychosocial factors and their complex interaction.
Of prime importance is to recognise the person with MS as a whole person in the context of lifestyle, values, roles, desires and relationships. Management depends on frank and open communication about sexual issues. Treatment of any underlying depression and anxiety may require medication and psychological counselling and the provision of ongoing monitoring and support. Counselling can help individuals to explore feelings and facilitate discussion in a respectful and professional way. You can identify negative emotions such as guilt, anger and resentment, see them in context, and work through them, in a non-judgemental environment. Here you can discuss topics, perhaps seen as too embarrassing to discuss alone, in an open and supportive atmosphere. Strategies for improving the situation, or adopting new ways of considering and developing sexuality, can be introduced.
Some people with MS may experience depression and/or anxiety, and medications prescribed for these conditions can affect sexual functioning. The drugs used to treat depression and anxiety belong to a family called ‘Selective Serotonin Reuptake Inhibitors’ (SSRIs). Commonly prescribed SSRIs include Fluoxetine, Sertraline, Fluvoxamine, Paroxetine, citalopram and Venlafaxine.
If you are taking any of these medications, you may experience:
Other, less common, side effects include secretion of breast milk, painful and persistent erection and irritation/inflammation of the head of the penis or the lining of the vagina.It is important to let your gP know if you are experiencing any of these side effects.
Sexuality is an important aspect of human life and must not be neglected when considering the impact of MS on an individual. If you have a partner, it is important to maintain open and honest communication with them regarding any sexual issues. However, difficult it may be, addressing problems and working together to find the solutions is the key to a quality relationship. Increasing awareness and acknowledgement of the effects of MS on sexuality has greatly improved the management and treatment options available for people with MS experiencing difficulties in this area. While this is often a difficult and sensitive subject, discussing sexual difficulties with your GP or neurologist is the first step to identifying effective strategies to manage any problems, and to support your need for sexual expression.
For more information please view our MSNZ Information Series booklet: Multiple Sclerosis and Sexuality and Intimacy