Your bladder can be affected in different ways by multiple sclerosis. It is estimated that more than 50 per cent of people with MS experience some bladder symptoms at some time. While bladder symptoms vary from person to person (as with most MS symptoms), there are broadly three types of bladder dysfunction: failure to empty, failure to store and combined dysfunction. You can overcome any embarrassment by seeking help. Discuss your bladder symptoms with your GP or neurologist. You need the diagnosis before the correct management techniques can be started. S/he can refer you to a continence advisor or urologist for the help you need. Your treatment could include bladder retraining, dietary changes, medication, using continence products or catheterisation. Urinary tract infections can largely be prevented, but if they do occur, they must be properly and promptly treated. If you plan to change your routine (e.g. going on a trip), anticipate problems and plan ahead. With good management, your bladder need not run your life.
The diagram shows the urinary tract. Urine is formed in the kidneys from a combination of excess fluid and impurities from the blood stream. Urine flows from the kidneys through the ureters to the bladder where it is stored before being released through the urethra. The bladder is a muscular bag. This slowly expands as urine collects, similar to the way a balloon expands as air is blown into it. The muscular part of the bladder is called the detrusor. At the opening of the bladder, where it meets the urethra, there is a muscle called the sphincter that remains contracted and closed between times of urination. The bladder and sphincter are normally under voluntary control, which means a person can control when they urinate. The bladder has a capacity of about 500mls before the urge to urinate is felt. The brain controls urination. Although the process is not clearly understood, the brain sends nerve impulses down the bottom of the spinal cord to the detrusor and sphincter. These impulses synchronise the contraction of the bladder and opening of the sphincter to ensure the urine proceeds in a coordinated way into the urethra.
How MS affects bladder function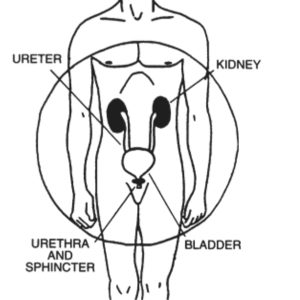
Multiple Sclerosis can cause damage to the nerve pathways that control the urinary system. This can affect the bladder’s ability to store urine, or the ability to empty itself of urine. In some cases these problems can occur at the same time.
Failure to store urine
Sometimes the mix up in messages from the nerve pathways mean the bladder detrusor muscle is overactive—contracting the bladder when only small amounts of urine are present.
This type of bladder dysfunction can cause:
Management
The idea is to relax the bladder detrusor muscle so that a normal amount of urine may accumulate before the urge to urinate is felt. This can be achieved by medication.
Failure to empty the bladder
Difficulty emptying the bladder usually occurs because the sphincter is spastic, meaning it is unable to relax easily and the bladder cannot complete its discharge into the urethra. As there is less pressure on the sphincter to relax, the bladder retains urine instead of discharging it. Conversely, the weakened detrusor may no longer be able to apply enough pressure to push the urine through the sphincter.
Problems with the sphincter and detrusor allowing the bladder to empty can cause:
Complications
Urine can ‘back up’ in both the kidney and the urinary tract. This built-up urine can crystalise into stones, or provide a breeding ground for infection. These issues must be treated.
Symptoms of possible infection or stones include:
There are some steps you can take to prevent infection:
Urinary tract infections are treated with antibacterial solutions available from pharmacists, but serious infections require antibiotic treatment from a GP. The chances of developing stones can be decreased through changes to food and liquid intake. Kidney and bladder stones predispose to infections and may need surgical treatment.
These solutions may require the input of a continence advisor, to whom your GP can provide a referral. Alternatively, the Urology Department of the local hospital can provide information on specialists in your area.
Continence products
Besides medication (discussed below) and catheters, there are a wide range of products and appliances available to assist with managing bladder problems. These are constantly being redesigned and re-evaluated by the manufacturers. Some products are available on prescription and some you have to buy. The best resource for products, availability and funding is Enable New Zealand. Alternatively, your Regional MS Community Support Staff will be able to provide one-on-one advice that reflects your situation . For men, a condom urinal may be a more suitable alternative to an indwelling catheter. A continence advisor can provide you the best advice here.
Medications
Bladder function tests
Tests of bladder function may include one or more of the following:
Fluids and diet
It is tempting to cut down on the amount you drink so that you will need to use the toilet less often, but please don’t do this.
A low fluid intake can lead to:
It is important to drink at least eight glasses of water a day. Some people find it helps to drink more during the day and less in the evening, to reduce the urge ‘to go’ in the night. It may be helpful to reduce tea and coffee as these are diuretics (substances that make you pass urine more frequently) but you will need to find an alternative. Alcohol increases the amount of urine formed, so drink in moderation.
It’s essential to maintain a balanced diet to ensure proper bowel function. Constipation can interfere with bladder function by:
A balanced diet should include plenty of fresh fruit, vegetables and fibre as well as plenty of fluid. Your Regional MS Community Support Staff or a registered dietician can all provide information on MS and diet.
Bladder Exercises
Simple exercises to strengthen the muscles that support your bladder are useful if you experience stress incontinence. Actions such as laughing or sneezing create pressure on weak bladder neck muscles. This causes urine to leak out. Exercises will not cure your bladder symptoms, but should strengthen your pelvic floor muscles and give you more control and time to reach a toilet. Identify the muscles of the pelvic floor by stopping the flow of urine, then restart it. The muscles you use are your pelvic floor muscles. Tighten the muscles while counting slowly to four, then release them. Do this four times every hour. Do it anywhere – sitting or standing, waiting for the bus – there is no need to set aside a special time. After several weeks you will probably feel stronger control.
It may be worth trying some exercises to ‘retrain’ your bladder. If you have a storage dysfunction and are passing urine frequently:
If you have an emptying dysfunction, use the clock and go at regular intervals, say two hours, even if you don’t have to. This will make sure you empty your bladder before it empties voluntarily.
Bladder massage
This is a commonly used technique that facilitates more complete bladder emptying. After as much urine has been emptied as possible, lean forward and apply pressure in a downward movement to the lower abdomen with both hands. It is necessary for men and women to sit firmly on the toilet seat to use this technique.
A thin tube is inserted into the urethra to drain the urine from the bladder. Although it sounds somewhat invasive, it is actually safe, effective, painless and easy to perform. Most people are advised to self-catheterise two or three times a day and perhaps before going to bed. Apart from the catheter itself, no other special equipment is needed and the bladder can be emptied as per usual in any toilet. Poor hand function, tremor and leg spasms can make this method more difficult, although poor eyesight does not prevent people from administering the system.
Intermittent Self-catheterisation
Self catheterisation can help to:
Provided the catheter tubes are kept clean and standard hygiene practices are followed there is very little chance of infection. After a period of self-catheterisation, the tone of the bladder muscles may improve, eliminating the need for this management technique.
You should talk to your health professional before self-catheterising.
Permanent or ‘Indwelling Catheters’
An indwelling catheter is a small tube that is passed into the bladder, most commonly through the urethra but sometimes through the abdomen. It is attached to a disposable bag that collects the urine. The tube and bag can be neatly strapped to the leg and worn discreetly under clothing.
Because the catheter is permanent, this increases the chances of infections and stones, thus it is not recommended for day-to-day bladder management. However, an indwelling catheter may be preferable when:
As an indwelling catheter can provide bacteria with a direct route to your bladder, care must be taken to minimise the risk of infection. Fluid intake should be at least three litres a day to irrigate the bladder and reduce this risk.
Suprapubic Catheter
A suprapubic catheter is a tube that is inserted through the abdominal wall into the bladder to drain urine into a bag. The bag has a tap and can be emptied into the toilet.
Suprapubic catheters are used as an alternative to urethral catheterisation, especially after trauma or surgery and to:
As with other types of catheters, care must be taken with the equipment. The catheter, tubing and drainage bag must be kept as clean as possible and hygienic practices followed when handling the equipment. A continence advisor will help with proper management.
There has been very little research carried out on the use of these therapies in dealing with bladder problems and, at the time of writing this booklet, virtually none that is specific to MS. However, some people have had good experiences and report success with a wide range of treatments. These include hypnotherapy, acupuncture, homeopathy and reflexology. Other therapies have, in their turn, all helped people and may well be worth a try, particularly if more conventional therapies have failed.
How do I manage at night?
Stay warm and dry when you are asleep, not only for comfort and a decent rest, but also to protect your skin and your bedding. Many continence products, including indwelling catheters, have special night versions designed to cope with periods of rest. You could consider a commode in the bedroom for bedtime use and a water resistant mattress protector will prevent damage to the bed.
How do I manage odour?
Any degree of incontinence can cause worries about smells, but the right advice from a continence advisor can allay these fears.
It is also important that your:
What can I do if THIS is affecting my sexual activity?
Most bladder issues can be managed effectively so that sexual ability and enjoyment is not compromised. It is important to seek advice from a continence advisor or sex therapist on this issue and your Regional MS Community Support Staff may also have some solutions. If you have a partner, it is crucial to discuss any worries with them so that mutual understanding can be achieved.
How do I cope with menstruation and bladder symptoms?
Menstruation can be an extra issue for women experiencing bladder problems. Women who are able to use tampons should continue to do so and most incontinence pads can also provide effective sanitary protection. Alternatively, a sanitary pad can be added to the continence pad for extra protection. Of course, regular changing of sanitary products is essential for skincare and to prevent odour. A continence advisor or your Regional MS Community Support Staff will be able to help with advice.
For more information please view our MSNZ Information Series booklet: Multiple Sclerosis and your bladder and bowel